Breaking news from the Diagnostic Center for Diseaseâ„¢ in Sarasota, Florida, identifies a previously underestimated risk that routine prostate biopsy performed to evaluate for prostate cancer spreads cancer cells and may be the reason that men have a recurrence of disease many years after the prostate was removed successfully with clear surgical margins. Traditionally, an ultrasound and prostate biopsy is commonly recommended and performed by Urologists when a patient presents with a prostate specific antigen (PSA) of 2.5 ng/ml or above. Men have been told for years that the procedure is safe and the only way to diagnose prostate cancer. While this paradigm represents the current standard, the protocol exposes far too many men to needless biopsies. Why should we perform biopsies preferentially on a male with an elevated PSA when the number one reason PSA rises is prostatitis, not prostate cancer? To be certain, many men will have a small cancer that is missed on biopsy based on the inability of this standard procedure to isolate a suspected lesion in question (sampling error). Regardless of the rationale for a biopsy, all men suffer the potential risk for bleeding, scarring, infection or sepsis from needless
“3.0 Tesla MRI-Spectroscopy predicts and confirms prostate cancerâ€
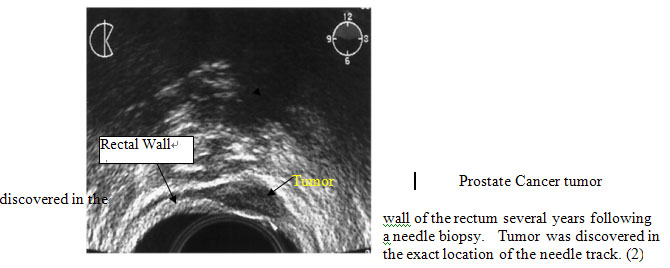
intrusion that has reportedly resulted in impotency and/or incontinence in some patients. A more important issue that is often not discussed between physician and patient involves the possibility of “needle trackingâ€; the very real possibility of spreading cancer cells beyond the prostate when a biopsy is performed. An extensive review of the literature confirms that once a needle penetrates the capsule of an organ, a phenomenon called “needle tracking†takes place. When the needle is withdrawn from the targeted organ, the chance of spreading cancer cells (when encountered) establishes itself while every puncture of the prostate adds to this risk. Despite the significance of this risk to the patient, physicians generally fail to acknowledge a process that allows cancer cells to lie dormant or incubate for up to 10 years or more regardless of the treatment rendered. In a 2 billion dollar prostate biopsy industry, the phenomenon of “needle tracking†takes place approximately 20-30 percent of the time. This coincides with the frequency that ultrasound and biopsy encounters a cancer, suggesting that 70-80 percent of biopsies are performed unnecessarily, while putting the patient at grave risk.
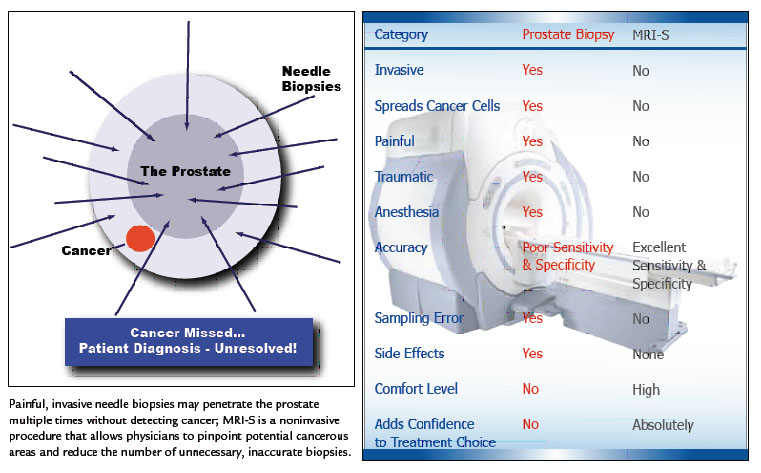
The solution to the conundrum of “needle tracking†may lie in improving our diagnostic skills through imaging, thereby, replacing random biopsies by a reduced number of biopsies targeted to the region of interest in the gland. The importance of developing an image based diagnosis is exemplified in research from the University of California at San Diego, where experts have discovered that biopsies of cancerous tissue enhance inflammation that hastens the progression of metastasis. According to Dr. Michael Karin, the lead author of their research scheduled for publication in the Journal, Nature – “proteins produced by inflammatory cells (stimulated by the biopsy) are the ‘smoking gun’ behind cancer metastasis. This is shocking information that patients need to know as they consider their diagnostic options. No longer can we promote biopsies as an innocuous event where no alternative exists.
A recent evaluation of data from patients noting a positive MRI-Spectroscopy (MRI-S) scan at the Diagnostic Center for Disease™ confirmed 75 percent of biopsies performed yielded a cancer, thereby, allowing many men without cancer to avoid a biopsy procedure altogether. In effect, a 3.0 Tesla MRI-S scan predicts and confirms the presence of prostate cancer almost 3 times more frequently than a randomized biopsy procedure. This is a quantum leap from the blind biopsy approach that yields a cancer in 20-30% of patients when an elevated PSA selects the patient population to be biopsied. Allowing an imaging system to predict the presence of prostate cancer enables the potential savings of millions of dollars to the healthcare industry. The secret to success highlights a 3.0 Tesla MRI-S scan, representing the most sensitive and specific diagnostic imaging modality for a prostate evaluation in the world, replacing substandard scanning procedures like PET scan, CAT scan and Prostascint scans. The MRI-S scan with a 3.0 Tesla resolution allows imaging of the entire prostate and pelvic region, thereby, creating a roadmap of disease recognition. This, subsequently, allows selective targeting of specific regions of interest for biopsy when indicated. In many cases, a biopsy is not recommended at all as no cancer is found. Furthermore, this methodology allows for fewer biopsies versus the “shot in the dark†12-24 core biopsy approach or the saturation biopsy (upwards of 80-90 biopsy cores), thereby, significantly minimizing risk to the patient. In the event a lesion is isolated, a specific protocol is implemented to prevent cells that escape the capsule from proliferating; in effect, causing cells to become weakened, disabled and die through a process called apoptosis.
This protocol is unique to the Diagnostic Center for Disease™. The Center’s success with the MRI-S scan is further magnified by de-selecting men with an elevated PSA who don’t have prostate cancer but rather have prostatitis, a non-bacterial inflammatory disease; the primary reason PSA rises. In these instances, the Center encourages the use of an internationally patented formula to decrease and/or normalize the PSA in patients without evidence of prostate cancer. While the literature suggests that all men will get prostate cancer if they live long enough, there is no reason to accelerate the diagnostic process or worse…undergo a premature biopsy, where the patient assumes considerable risk. To reiterate, a 3.0 Tesla MRI-S scan creates a roadmap to guide targeted biopsies to the specific region of interest while avoiding areas that fail to exhibit the “fingerprint†of disease. At the Diagnostic Center for Disease™, physicians recognize that better imaging enables an improved opportunity to diagnose disease while ensuring a better, more predictable outcome.
A recent case of a 71-year-old man illustrates the benefit of the 3.0 Telsa MRI-S scan. In 1997, the PSA was measured at 3.7 ng/ml. Presumed to be in normal range; the PSA was not tested again until 2001, when it was 7.2 ng/ml, well above, the traditionally recognized 4.0 ng/ml level for concern. A biopsy using a traditional gray-scale ultrasound evaluation resulted in eight negative cores. The following year, the patient’s PSA was 11.5 ng/ml. This time, in addition to the gray-scale ultrasound, the color flow doppler (CFD) ultrasound was utilized to isolate areas of blood flow, important to prostate cancer growth. Despite the use of CFD to target areas of interest, the biopsy results were once again negative. Frustrated, the patient turned to the 3.0 T MRI -S scan. Despite a lack of evidence for cancer on the physical examination of the prostate, the scan located a discreet, well-defined 4.5 mm lesion deep within the peripheral zone of the mid-prostate on the left side. Subsequently, five targeted biopsies identified an aggressive cancer. Having established that the cancer was organ confined with no evidence of spread to the surrounding tissue, the patient was now able to focus on appropriate treatment options.
“Men who have an elevated PSA and want to avoid an unnecessary prostate biopsy now have an alternative to a blind biopsyâ€, states Ronald E. Wheeler, M.D., the Medical Director at the center. Additionally, men who want a second opinion when the previous biopsy was negative, can now go to the only imaging center in the world that is dedicated exclusively to the diagnosis and treatment of prostate disease. To learn more, call the center today at (877)-766-8400 or visit online at www.mrisusa.com.
Diagnostic Center for Diseaseâ„¢
1250 S. Tamiami Trail
Suite One North
Sarasota, FL 34239
(941) 957-0007 – www.mrisusa.com
References:
1. Moul, J.W., Bauer, J.J., Scrivastava, S., Colon, E., Ho, C.K., Sesterhenn, I.A., etal.: Perineal seeding of prostate cancer as the only evidence of clinical recurrence 14 years after needle biopsy and radical prostatectomy: molecular correlation. Urology, 51: 158, 1998
2. Koppie, T.M., Grady, B.P., Shinohara, K.: Rectal wall recurrence of prostatic adenocarcinoma. Journal of Urology, 168: 2120, 2002
3. Bastacky, S.S., Walsh, P.C., Epstein, J.I.: Needle biopsy associated tumor tracking of adenocarcinoma of the prostate. Journal of Urology, 145: 1003, 1991